| 2004 |

|
YEAR BOOK |
University College Dublin
|
Neutrophil migration in the lung: an important target for therapies in inflammatory lung disease
|
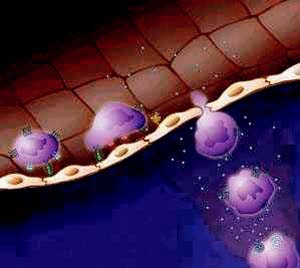
The neutrophil is a white blood cell that defends the body when infection attacks. The neutrophil patrols the body with a 24-hour surveillance system, circulating in the blood stream and responding to alarm signals generated when infection strikes. When the neutrophil detects an alarm signal, it mobilises to move from the bloodstream to the site of infection, where it swallows the invading microorganisms and restores the normal environment. The neutrophil works in concert with other white blood cells in this manner to maintain healthy tissues throughout the body. This cycle of infection and resolution of infection is called inflammation. Inflammation is one of a host of effective defence mechanisms that ensures health and longevity.
In response to an infectious signal, messages are sent from protein to protein within the neutrophil in order to mobilise it to fight the infection. Part of this process involves activating particular proteins that will allow the neutrophil to move to the site of infection, where it can then swallow the invading microorganism. This process of relaying messages within the cell is called signal transduction. Another critical part of the neutrophil response to an infectious signal is to switch on the expression of certain genes to produce proteins that are essential for the resolution of infection.

Learning more about the messages that are relayed within the neutrophil as it migrates will result in a clear understanding of the proteins involved in the migratory pathways for many infectious signals. Armed with this information, targets for therapeutic intervention in inflammatory lung diseases can be identified. We then move a step closer to the lung-specific reduction of neutrophil migration in inflammatory lung disease.
* Eavan Daly was one of the winners in AccesScience '04 held in UCD in May 2004. Eavan works in Dr Clare O'Connor's Group. This is a summary of her presentation.
Contact: Eavan Daly, Department of Medicine and Therapeutics, Conway Institute, University College Dublin;
Tel: (01) 7166752; E-mail: [email protected] ; Web: http://www.ucd.ie/conway