| 2004 |

|
YEAR BOOK |
Cork Cancer Research Centre & University College, Cork
|
Enhancing delivery and efficacy of anti-cancer drugs
|

|

|
The Cork Cancer Research Centre (CCRC) provides infrastructural resources and facilities to researchers focused on combating cancer. The objective of the Centre is to develop preventative measures and/or therapies for those patients who will benefit most from them. The Centre is unique in its multidisciplinary approach in addressing cancer research challenges, representing the physical manifestation of long-term collaborations between researchers based in University College Cork (UCC) and its Associated Teaching Hospitals. Physically, the CCRC is located in both the Mercy University Hospital, Cork and at the BioSciences Institute on the UCC campus. Through provision of financial support for complementary research programmes, the CCRC is also represented by scientists and physicians based in nearby university departments and other research centres.
Core activities at the CCRC include the study of genetic events associated with solid tumours and leukaemia, DNA methylation in cancer, detection of metastatic (secondary) disease, and the screening of 'at risk' individuals at a colon cancer prevention screening clinic based at the Mercy University Hospital in partnership with Dublin's Mater Hospital, all funded through the Irish Cancer Society and the Health Research Board. Additional funding for the centre has been obtained from the European Commission, the Higher Education Authority, Enterprise Ireland, corporate sponsors and philanthropists.

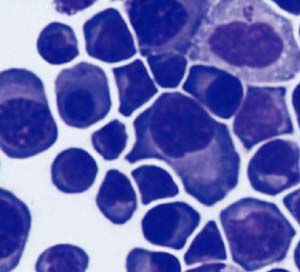
(A) introduction of therapeutic drugs, |
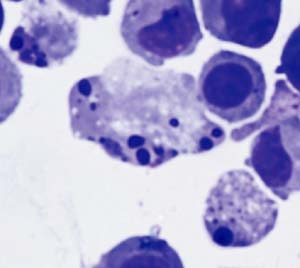
(B) the induction of apoptosis (cell death) |
In a complementary initiative, the efficiency of anticancer drugs is being enhanced. Investigators at the CCRC, funded by the Irish Cancer Society and the Higher Education Authority, are examining the effects of treating human-derived oesophageal, colon, bladder, kidney and breast cancers with well-defined 'cocktails' of therapeutic and preventative pharmaceutical agents. The influences that these combinations exert on the growth rates of the tumours under laboratory conditions are, in some cases, dramatic (Figure 2) and may indicate new uses (or dosages) for certain drugs.

Contact: Professor Gerald O'Sullivan (Director) or Dr Colum Dunne (General Manager),
Cork Cancer Research Centre, Mercy University Hospital & BioSciences Institute, University College, Cork;
Tel: +353-(0)21-4271971; E-mail: [email protected] ; Web: www.ccrc.ie