| 2004 |

|
YEAR BOOK |
Trinity College Dublin
|
Novel immunosuppressive compounds to treat asthma
|
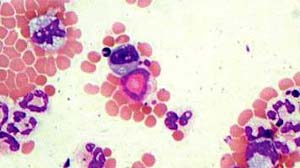
A variety of agents can contribute to asthma, but a major factor is immediate hypersensitivity to allergens such as pollens and dust mites. Specific ImmunoglobulinE (IgE) antibody-antigen interaction is a major trigger mechanism for the release of a number of mediators from mast cells, including histamine, leukotriene-D4, prostaglandin D2, IL-4 and TNF-a. Although histamine can cause bronchoconstriction, it is probably less important than leukotriene D4, a primary bronchoconstrictor. In many cases, a delayed increase in bronchial hyper-reactivity develops to common allergens and is known as extrinsic asthma. Another form of obstructive airways disease is intrinsic asthma, which differs in that it does not appear to involve hypersensitivity to stimulants, or high levels of circulating IgE antibody.
Both types of asthma may be treated by a variety of drugs, including cromoglycate, bronchodilators and inhaled steroids. However, intrinsic asthma is more difficult to control, with some sufferers resistant to inhaled and systemically administered steroids (the latter with greater potential for adverse effects). Cyclosporin can treat steroid-resistant intrinsic asthma, but is often considered a last resort drug due to its severe toxicological profile. Although there are other immunosupressants available, they are also not without their side effects.
This project involves establishing a novel murine model of intrinsic asthma. Several novel immunosupressants generated in this group will be evaluated by examining their effect on eosinophilia and cytokine profiles in the model. It is hoped that promoting the involvement of Th1 lymphocytes in the developing immune response will duplicate the cytokine profile seen in intrinsic asthmatics. However, the distinction between Th1 and Th2 responses is not so clear anymore. Numerous animal models suggest that Th1 cells promote pro-inflammatory actions, while Th2 cells are anti-inflammatory. Recent reports concerning the EAE/MS model contradict this theory, with Th2 cells found to induce brain inflammation in immunodeficient mice and TNF-a, a major proinflammatory cytokine, may be protective in this model. Current research involving the role of T regulatory cells in the immune system is adding complexity.
This study investigates novel immunosuppressants in asthma while keeping the complexity of the immune system in mind at all times.
Contact: Brendan McHale, School of Pharmacy, Trinity College Dublin;
E-mail: [email protected]